(+27) 82 511 8212
What is Facial Palsy?
Facial palsy refers to weakness or paralysis of the muscles in the face, usually caused by a problem with the facial nerve. This nerve carries messages from the brain to the facial muscles, telling them how and when to move. When the nerve is damaged or compressed, often due to swelling, those messages can’t get through, and the muscles stop working properly. As a result, one side of the face may droop or movement of the eye(s), mouth and/or other areas of the mouth is affected.
You can think of the facial nerve like a train track carrying messages from the brain to the muscles. If something blocks the track, for example a fallen tree, the train (or message) cannot get through. Once the blockage is cleared, the trains can run again and the messages reach the muscles. At this time, muscle movement may gradually return.
The facial nerve is made up of many small fibers (called axons) grouped together, much like wires inside a cable. How the nerve recovers depends on the type and extent of damage. Facial nerve injuries can vary in severity, and the extent of the damage plays a major role in how well and how quickly someone might recover.
Facial nerve injuries are typically grouped into three main categories, ranging from mild to severe:
-
Mild Injury (Neuropraxia / First-Degree Injury): This is the least severe type of facial nerve damage. The nerve is temporarily “stunned” or bruised, but not permanently harmed. Signals from the brain are temporarily blocked, which leads to weakness or paralysis. Most people begin to recover within a few weeks, and full recovery often occurs within 6 to 8 weeks. In many cases, therapy isn't required, though some may benefit from a session or two for advice and reassurance.
-
Moderate Injury (Axonotmesis / Second-Degree Injury): In this type of injury, the inner fibres of the nerve are damaged, but the outer protective layer remains intact. The nerve must regenerate, growing at a slow rate of about one millimetre per day. Because of this, visible signs of recovery may not appear until around 4 months after the injury. Recovery can take several months, and while it is often good, it may not be complete. Early facial therapy is strongly recommended to support healing, improve muscle coordination, and help prevent unwanted movement patterns such as synkinesis.
-
Severe Injury (Neurotmesis / Third-Degree Injury): This is the most serious form of facial nerve damage. The nerve may be significantly disrupted or even completely severed, often due to trauma or surgery. In these cases, natural recovery is limited, and surgical repair is usually necessary to restore some degree of function. Even with surgery, recovery tends to be slower and often incomplete. Ongoing specialist facial therapy is essential to support rehabilitation and maximize outcomes.
Understanding the type and degree of facial nerve injury is crucial for setting realistic expectations and guiding the appropriate treatment plan.
Facial palsy can affect different areas of the face and to different degrees; sometimes just the lower face, sometimes one entire side, and occasionally both sides. Recovery depends on the severity of the nerve damage, but with the right treatment and support, many people experience improvement in their facial movement and function over time.
How does the facial nerve work?
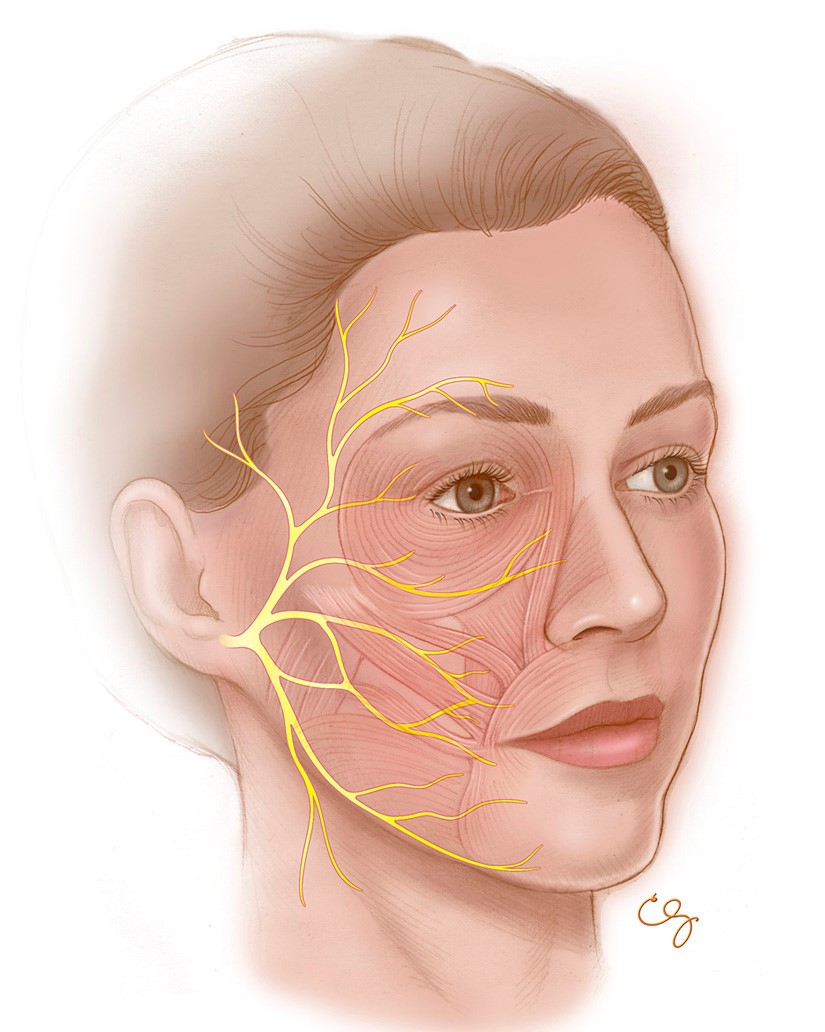
Each side of the face is controlled by its own facial nerve, so if one side is affected — for example, the left facial nerve — only the muscles on the left side of the face will be impacted. The facial nerve starts in the brain and travels through the skull to just in front of the ear, where it divides into five main branches. These branches control the muscles used for facial expressions.
In addition to muscle movement, the facial nerve also helps with other important functions. It plays a role in producing tears and saliva, helps us detect certain tastes, and even helps to dampen loud sounds by controlling a tiny muscle in the ear called the stapedius. When the nerve isn’t working properly, these functions can also be affected.
What functions do the facial nerves perform?
-
Raising the eyebrows
-
Closing the eyes
-
Frowning
-
Open mouth smiling
-
Closed mouth smiling
-
Pouting
-
Lifting top lip
-
Pulling lower lip down
-
Sticking bottom lip out
-
Pulling jaw and corners of mouth gently down
-
Wrinkling nose
Causes of facial palsy
While Bell’s palsy is the most widely recognized cause of facial paralysis, there are actually many different reasons why someone might develop facial palsy. The appropriate treatment and the outlook for recovery can vary significantly depending on the underlying cause.
Some of the key causes include:
-
Bell’s palsy – A condition where the exact cause remains unknown, though it is often linked to viral infections. It is considered idiopathic, meaning no specific reason has been definitively identified.
-
Viral infections – Certain viruses can directly affect the facial nerve. One example is Ramsay Hunt syndrome, which is caused by the varicella-zoster virus (the same virus responsible for chickenpox and shingles).
-
Surgical factors – Facial palsy can occur as a result of surgery, particularly during operations near the facial nerve, such as the removal of an acoustic neuroma, facial nerve tumours, or surgery on the parotid gland.
-
Bacterial infections – Conditions like Lyme disease or complications from a middle ear infection can lead to inflammation or damage to the facial nerve.
-
Neurological disorders – Some disorders of the nervous system, such as Guillain-Barré syndrome or Neurofibromatosis type 2 (NF2), can involve or affect the facial nerve.
-
Trauma – Physical injuries to the head, skull, or face, including fractures, can damage the facial nerve and lead to paralysis.
-
Birth-related injuries – Facial palsy may occur in newborns due to complications during delivery, such as the use of forceps or certain types of fetal positioning.
-
Congenital causes – Some individuals are born with underdeveloped facial nerves or muscles, which can result in facial palsy from birth.
-
Genetic syndromes – Rare inherited conditions, such as Moebius syndrome or CHARGE syndrome, can include facial palsy as part of their set of symptoms.
-
Stroke – Although strokes can result in facial weakness or paralysis, the mechanism is different. In this case, the facial nerve itself isn’t damaged; rather, the part of the brain that controls facial movement is affected, disrupting the messages sent to the nerve.
Understanding the specific cause of facial palsy is important in guiding the most effective treatment approach and predicting how recovery may progress.
How Facial Palsy Affects Individuals
Facial palsy can have a wide range of effects, both physical and emotional. Although it is often assumed to be purely cosmetic, the condition can impact many aspects of daily life.
Symptom Onset and Diagnosis
Symptoms of facial palsy may appear suddenly, sometimes overnight, or may develop gradually over days, weeks, or even months. Regardless of how quickly symptoms appear, it is important to seek medical advice early to identify the cause and begin appropriate treatment. Accurate diagnosis is crucial for managing the condition effectively.
Common Symptoms
Facial palsy typically affects one side of the face, though in rare cases, both sides may be involved. Common symptoms include:
-
Muscle weakness or paralysis on the affected side, often involving the brow, eye, cheek, and mouth
-
Difficulty with facial movements, such as smiling, blinking, frowning, or raising an eyebrow
-
Loss of facial sensation (in cases where other nerves, like the trigeminal nerve, are also affected)
-
Eye issues, including incomplete eyelid closure, dryness of the eye, tearing, irritation, or light sensitivity
-
Changes in mouth function, such as drooping, drooling, trouble eating, drinking, speaking, or brushing teeth
-
Altered taste and saliva production
-
Ear symptoms, such as pain, hearing changes, or increased sensitivity to sound
-
Nasal symptoms, including difficulty flaring the nostril or a runny/stuffy nose
Any sudden weakness involving both the face and limbs may indicate a stroke and requires urgent medical attention.
Functional Challenges
Facial movement is essential for non-verbal communication. People with facial palsy may struggle with basic expressions like smiling or frowning, which can affect how they interact socially and how others perceive them.
-
Eye care becomes more difficult due to reduced blinking and eye closure, increasing the risk of dryness, irritation, and vision problems.
-
Hearing may be affected due to dysfunction of the stapedius muscle, which normally helps regulate loud sounds. Some people may find their own voice or everyday sounds uncomfortably loud.
-
Eating and drinking can be challenging due to weakness in the lips and cheeks, leading to difficulty retaining food, drooling, or biting the inside of the mouth.
-
Oral health may suffer due to reduced saliva, which protects against tooth decay. Tooth brushing can be challenging, and denture fit may change.
-
Speech may be less clear because of reduced lip and cheek muscle tone, making it harder to pronounce words or speak with confidence.
-
Pain is not usually caused by damage to the facial nerve itself, but some conditions (e.g., Ramsay Hunt syndrome) can cause significant discomfort.
-
Spasms and synkinesis (i.e. abnormal movements or twitching) may develop during recovery. These involuntary movements can affect facial control and may require specialist therapy to manage.
Emotional and Social Impact
Facial palsy often affects self-esteem and emotional well-being. Changes in appearance, speech, and expression can lead to self-consciousness, anxiety, or depression, regardless of the severity of physical symptoms. Some individuals may avoid social situations or feel isolated due to fear of judgment.
Children may be especially vulnerable to teasing or exclusion as they become more aware of differences. Adults may also face stigma, such as inappropriate comments or social discomfort.
Forming relationships can be harder when facial expressions are limited. Smiling, often a key part of connecting with others, may be difficult, leading to misunderstandings or feelings of disconnection. Some individuals may alter how they socialize; they avoid eye contact, hide their smile, or turn their face away; all which can unintentionally make them seem withdrawn or unfriendly.
Despite these challenges, many people with facial palsy adapt by developing alternative ways to communicate, such as using gestures, eye contact, and vocal expression. Support from loved ones, therapy, and education about the condition can make a significant difference.
Coping and Support
Emotional support is just as important as physical recovery. Building self-confidence, developing positive coping strategies, and seeking psychological support (e.g., cognitive behavioural therapy) can help individuals manage mood changes and social anxiety.
Support for children, education for peers, and open conversations with family and friends are vital to reducing stigma and improving quality of life.
Facial Therapy
Why should I start facial therapy early?
Beginning facial therapy early offers several important advantages. When the facial nerve is damaged or recovering slowly, the muscles may start to develop unhelpful movement patterns. Over time, these patterns can lead to longer-term complications, such as synkinesis (involuntary or abnormal facial movements). Studies have shown that early intervention with facial therapy can reduce the likelihood of these issues and support more effective facial movement earlier in the recovery process.
Stages of Facial Palsy Recovery
Recovery from facial palsy typically progresses through three stages:
-
Flaccid Paralysis: At this early stage, there is a complete loss of movement on the affected side of the face. The muscles appear slack, and the eye on the affected side may remain open due to the inability to blink or close it fully.
-
Paresis: As the facial nerve starts to heal, small, subtle movements begin to return. These changes can be gradual and sometimes difficult to notice at first, as the nerve slowly re-establishes connections with the facial muscles.
-
Synkinesis: In this stage, movement returns but is often uncoordinated. Involuntary muscle contractions may occur during voluntary actions, such as the eye closing when trying to smile. The face can feel tight or stiff, and muscle overactivity may cause discomfort.
Understanding the Difference Between Facial Paralysis and Synkinesis
Facial paralysis and synkinesis are often confused, but they represent different stages and types of facial nerve dysfunction.
Facial paralysis refers to a complete lack of movement on one side of the face. The muscles appear inactive or lifeless, and this typically occurs in the early stages following the onset of the condition.
Synkinesis, by contrast, tends to develop later in the recovery process. As the facial nerve begins to heal, it may form incorrect connections, causing movements to become misdirected. This means that when a person tries to perform one facial action, like smiling, another unintended movement, such as the eye closing, may occur at the same time.
Each stage of recovery requires a tailored therapeutic approach. Specific retraining techniques are used depending on the current phase to support effective and appropriate rehabilitation.
What if I have had facial palsy for a long time? Can I be helped?
Specialist facial therapy can be beneficial for everyone affected by facial palsy, regardless of whether the condition has been present for weeks, months, years, or even from birth. We have worked with patients living with facial palsy for over a decade who have still experienced significant improvements through therapy.
Why should I not go to a general therapist?
Facial rehabilitation is not typically covered in undergraduate university training, so general therapists often lack specialized knowledge in this field. As a result, they may recommend exercises and treatments that are unsuitable, as rehabilitation of the face requires different approaches than those used for other parts of the body.
Specialist facial therapists undergo additional postgraduate education focused specifically on facial rehabilitation. The majority of these experts are members of a professional organization dedicated to facial therapy and continue to further their knowledge and expertise in light of the latest developments and research.
What to Expect When You Begin Therapy with Us
Once you get in touch, we will send you an initial intake form along with some assessment questionnaires to complete and return before your first appointment.
Your initial consultation will take place in person (if you are based in the Cape Town area), or online via Zoom or Microsoft Teams. A secure link will be provided to you by your therapist ahead of the session.
Facial therapy involves a detailed evaluation of your facial muscle movement and muscle length. During the first session, we will also explain the underlying causes of your symptoms and help you build a clear understanding of your condition, so you can manage it confidently and effectively.
Please set aside up to two hours for your first appointment. This allows your therapist enough time to carry out a full assessment, answer your questions, and guide you through your personalised home programme.